Economically vulnerable communities in Shelby County are still experiencing a lack of health-care resources, according to findings from the area’s two largest hospital systems.
Though the two systems’ methodologies differed slightly, hoards of gathered data coupled with community feedback by Baptist Memorial Health Care Corporation and Methodist Le Bonheur Healthcare tell the same tale: It’s harder for those in poor neighborhoods to get access to health care.
Specifically, Memphis rests below the national baseline for access to medical care and maternal and infant/child health-care access and exceeds the national average in mortalities due to adult cancer, heart disease, addiction, and gun violence.
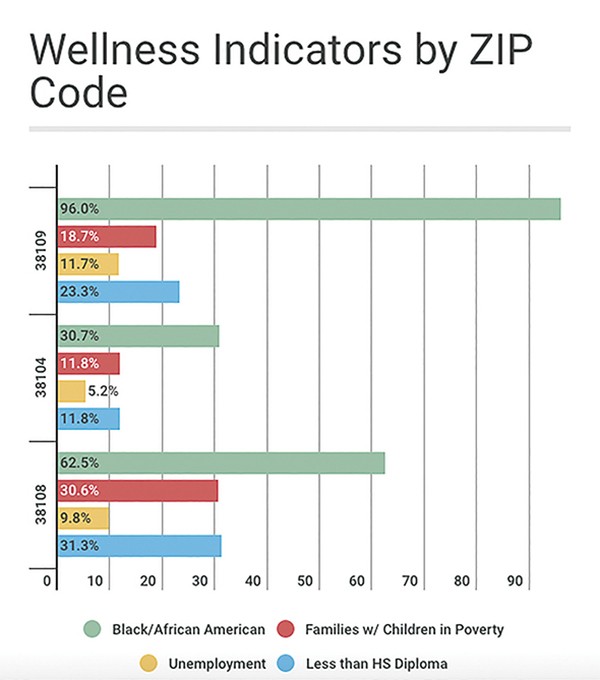
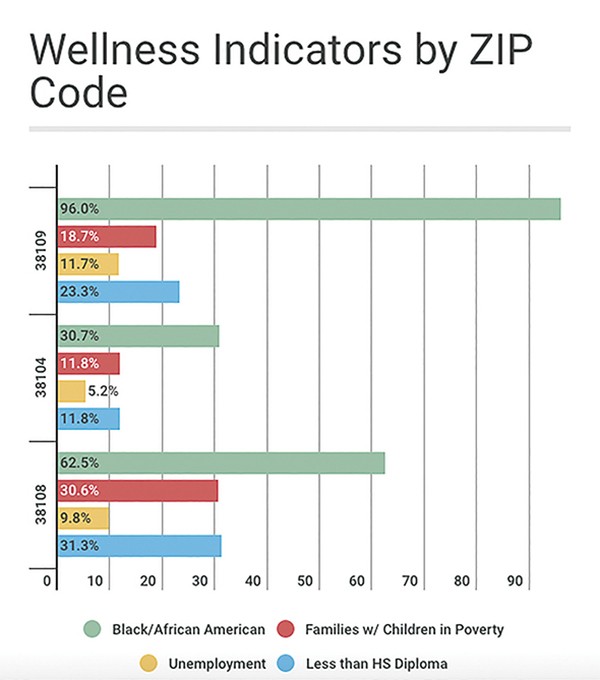
The lack of care and excess of disease in the poorest ZIP codes affect Memphis’ wellness rates as a whole community when compared nationally. But more in-depth analysis by the hospital systems shows familiar themes that have been long present in Memphis.
The affected communities are all majority black and impoverished, according to the studies. Resources needed for optimal health — such as reliable public or private transportation, education, health insurance, access to fresh foods, and employment — fall well below the rest of the city, state, and country.

A scene from the 38109 ZIP code
Two of the poorest ZIP codes in the country, 38108 and 38109, are identified as especially vulnerable in the reports. Low levels of education, health-care access, and employment have sent the poverty levels for these communities soaring well above the national average.
Findings from the reports show that the primary source of health care in these communities is the criminal justice system, particularly for residents suffering from mental illness and addiction. In addition to the financial strain on the Shelby County jail system, hospital emergency rooms are also overtaxed as they are often used as a primary care provider for Memphis’ poorest.
Across Memphis, there has been a sharp increase in deaths related to behavioral and mental health disorders. The age-adjusted death rate due to mental health increased in Shelby County from 18.3 per 100,000 in 2004 to 49 per capita in 2013.
Baptist and Methodist’s findings do point to some areas of progress. While access to prenatal care is still a need in Memphis, some advancements have been made in the declining number of teen pregnancies, infant mortalities, and overall maternal health.
Memphis once had the highest infant mortality rates in the country, but through increased prenatal care and education, the city has seen that rate drop from more than 13 deaths per 1,000 live births in 2008 to 8.2 deaths per 1,000 live births in 2016.
To combat the many critical needs in the overall landscape of Memphis, both hospitals have pointed to community partnerships between hospital systems and community-oriented nonprofits to increase health-care access and education.
Though there are ZIP codes in Memphis that endure economically related health deficiencies more than other ZIP codes, the burden of inadequate health-care access is felt by all taxpayers as many Memphians are forced to rely on public hospitals and jails for their health-care needs.
 Courtesy of Comunidades Unidas en Una Voz
Courtesy of Comunidades Unidas en Una Voz 
 Micaela Watts
Micaela Watts 

 Google Maps
Google Maps